What causes a wound to turn black?
Generally, darkening of a wound may be caused by factors such as pigmentation, blood scab formation, skin necrosis, wound infection, or diabetic foot. If discomfort occurs, timely medical attention is recommended. Detailed explanations are as follows:
1. Pigmentation
During the healing process, skin cells regenerate and repair themselves, which may lead to pigmentation and cause the wound area to darken. This is a natural physiological reaction and generally does not cause adverse effects to the body. Avoid prolonged exposure of the wound to sunlight to reduce pigmentation caused by ultraviolet radiation.
2. Blood Scab Formation
After a wound bleeds, red blood cells in the blood coagulate and form a blood scab covering the wound surface. The color of the scab is usually dark, which may give the impression that the wound has turned black. Prompt hemostasis and proper wound care are necessary after injury. Keep the wound clean and avoid forcibly removing the scab; allowing it to fall off naturally can help reduce the appearance of darkening.
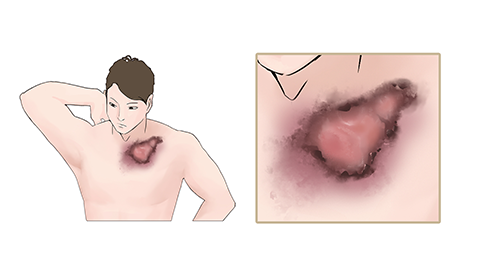
3. Skin Necrosis
Skin necrosis typically occurs due to poor blood circulation at the wound site, leading to hypoxia and ischemia of the skin tissue and ultimately necrosis. The necrotic tissue darkens, appearing black or dark brown. Accompanying symptoms may include wound pain and swelling. Patients should follow medical advice to apply medications such as erythromycin ointment, mupirocin ointment, or recombinant human epidermal growth factor gel for treatment.
4. Wound Infection
Wound infection may occur if the wound is not properly managed, allowing bacteria to invade and multiply, causing infection. The infected area may darken and be accompanied by symptoms such as elevated body temperature, fatigue, and fever. Under a doctor's guidance, patients may use medications such as amoxicillin capsules, cefradine capsules, or levofloxacin hydrochloride capsules for treatment.
5. Diabetic Foot
Diabetic foot occurs in patients with diabetes due to elevated blood glucose levels that cause peripheral neuropathy and vascular disease, making the skin on the feet prone to injury and difficult to heal. The wound may darken and may be accompanied by ulcers, necrosis, and reduced sensation. Patients may use medications such as metformin tablets, gliclazide modified-release tablets, or recombinant human insulin injection as advised by a physician.
In daily life, it is important to keep wounds clean and dry to avoid infection; control blood sugar levels to prevent complications such as diabetic foot; and undergo regular physical examinations to detect and treat underlying conditions such as vasculitis promptly.





