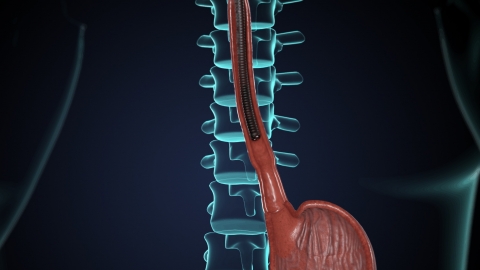
What issues can be detected through a gastroscopy?
Generally, gastroscopy can detect conditions such as gastritis, esophagitis, gastric polyps, gastric bezoars, and reflux esophagitis. If discomfort symptoms occur, it is recommended to seek timely diagnosis and treatment at a reputable hospital. Detailed analysis is as follows:
1. Gastritis
Gastroscopy allows direct observation of the color, texture, and morphology of the gastric mucosa. In cases of gastritis, the gastric mucosa often shows changes such as congestion, edema, and erosion. For example, chronic superficial gastritis may present with mucosal redness and roughness, while atrophic gastritis is characterized by pale mucosal color, flattened or even disappeared folds, and local areas may be accompanied by granular elevations or visible mucosal blood vessels.
2. Esophagitis
Gastroscopy can clearly display mucosal lesions in the esophagus. In patients with reflux esophagitis, the lower esophageal mucosa may show linear or patchy congestion and erosion; severe cases may develop ulcers. Fungal esophagitis presents as a white or yellow-white pseudomembrane covering the esophageal mucosa surface, beneath which the mucosa appears congested and rough after wiping.
3. Gastric Polyps
Under gastroscopy, gastric polyps typically appear as elevated lesions protruding into the gastric cavity from the mucosal surface, varying in size and shape. Common hyperplastic polyps are mound-like with a smooth surface, while adenomatous polyps often have stalks and may show surface congestion and erosion. Gastroscopy enables direct observation of the number, location, and morphology of polyps.
4. Gastric Bezoars
Gastroscopy can reveal irregularly shaped masses in the stomach with a hard texture, usually dark brown or yellow-green with a rough surface. Gastric bezoars often form when foods rich in tannic acid react with gastric acid, and gastroscopy can observe the relationship between the bezoar and the gastric mucosa.
5. Reflux Esophagitis
As described above for esophagitis, gastroscopy is an important method for diagnosing reflux esophagitis. Endoscopic findings include congestion and edema of the lower esophageal mucosa; severe cases may show longitudinal erosions or ulcers, typically distributed along the long axis of the esophagus.
Patients must fast for 6-8 hours before undergoing gastroscopy to avoid food residue affecting visualization. For two hours after the examination, food and water should be withheld until the numbing sensation in the throat subsides, after which warm, cool liquid or semi-liquid foods can be consumed to avoid irritating the mucosa with spicy or hot foods. If severe abdominal pain, hematemesis, or melena occurs after the exam, immediate medical attention is required to rule out complications such as gastrointestinal perforation or bleeding.







