What should be done if a wound is infected with amoebas?
Amebic wound infections generally require management through wound debridement, drug therapy, complication management, nutritional support, and rehabilitation nursing. If any abnormalities occur, prompt medical attention is recommended. Detailed analysis is as follows:
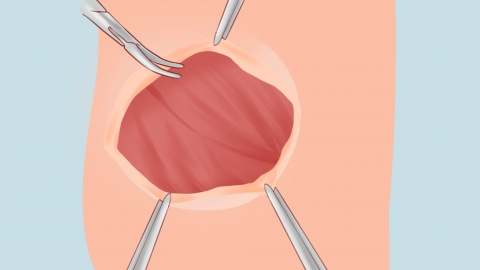
1. Wound Debridement: Immediately and thoroughly irrigate the wound with normal saline to remove necrotic tissue and secretions. When necessary, apply wet dressings using chlorhexidine acetate solution or 1:5000 potassium permanganate solution to disrupt the living environment of the amebas. During debridement, ensure deep wound exposure and remove all visible contaminants to minimize parasite residue.
2. Drug Therapy: Under a physician's guidance, administer systemic nitroimidazole medications such as metronidazole tablets to inhibit amebic DNA synthesis. Locally, apply metronidazole gel or chlorhexidine gluconate ointment to directly kill parasites on the wound surface. Change dressings daily to maintain adequate medication concentration in the wound.
3. Complication Management: If the infection spreads, causing sepsis or abscesses in adjacent tissues, combine antibiotic therapies such as ceftriaxone sodium injection, levofloxacin hydrochloride injection, or penicillin sodium injection to control secondary bacterial infections. Perform ultrasound examinations to determine the extent of abscesses and, if necessary, perform needle aspiration or incision and drainage to prevent further infection spread.
4. Nutritional Support: Provide a high-protein, high-vitamin diet including lean meats, eggs, and fresh fruits and vegetables to enhance immune function. If the patient has poor appetite, administer intravenous amino acids and fat emulsions to supplement nutrition, promoting wound healing and tissue repair.
5. Rehabilitation Nursing: Maintain wound dryness and cleanliness, regularly change dressings, and monitor healing progress. Avoid exposing the wound to water or contact with contaminants. After symptom relief, gradually increase physical activity, avoid pressure or tension on the wound, and schedule regular follow-up tests for complete blood count and wound exudate pathogens to ensure complete eradication of infection.
In daily life, avoid exposing wounds to suspicious contaminants such as sewage or soil. Clean wounds promptly with soap and water after injury and disinfect appropriately. If abnormal redness, discharge, or increased pain occurs at the wound site, seek immediate medical attention. Do not attempt self-treatment to prevent delayed treatment.