Is hemolytic jaundice in newborns serious?
Generally, the severity of neonatal hemolytic jaundice varies depending on the rate of hemolysis and bilirubin levels. When hemolysis is mild and bilirubin levels are manageable, the condition is not severe. However, when severe hemolysis causes a sharp rise in bilirubin levels or complications occur, the situation becomes serious. If any abnormalities are noticed, timely medical consultation is recommended. Detailed analysis is as follows:
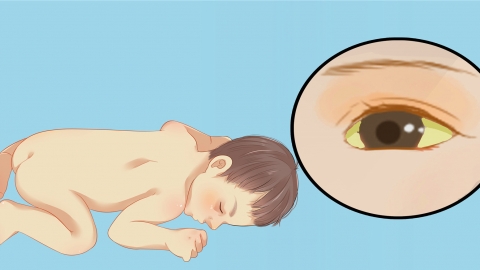
If neonatal hemolytic jaundice is caused by mild ABO blood group incompatibility, the hemolysis progresses slowly, and the increase in bilirubin levels is small, not exceeding dangerous thresholds. The infant remains in good general condition, feeds normally, and shows no signs such as lethargy or refusal to feed. With treatments like phototherapy, bilirubin levels can drop rapidly, the condition can be controlled within a short time, and the impact on the infant's health is minimal, with a good prognosis.
When neonatal hemolytic jaundice is caused by Rh blood group incompatibility, the hemolytic reaction is intense, and bilirubin levels rise sharply within a short time, exceeding safe ranges. Bilirubin encephalopathy may develop, presenting symptoms such as seizures, opisthotonus, and hearing impairment. At this stage, the condition is severe and may cause irreversible damage to the nervous system or even threaten life. Emergency blood exchange therapy is required, and even with treatment, long-term complications may remain.
When a neonate develops hemolytic jaundice, bilirubin levels and physical status should be closely monitored. Phototherapy or blood exchange therapy should be strictly administered under a doctor's guidance. During treatment, attention should be paid to maintaining body temperature and proper feeding to ensure timely and effective intervention for the newborn.






