How to Determine if It Is Vasculitis
Generally, determining whether a condition is vasculitis involves a comprehensive analysis of typical symptoms, affected areas, laboratory tests, imaging findings, and pathological examinations. Specific factors include manifestations of the skin and mucous membranes, signs of multi-system involvement, abnormal inflammatory indicators, vascular imaging changes, and results from pathological biopsies. Detailed analysis is as follows:
1. Skin and mucous membrane manifestations: Vasculitis often presents with symptoms on the skin and mucous membranes, such as purpura, erythema, nodules, and ulcers. Purpura typically appears as purple-red petechiae or ecchymoses that do not fade upon pressure, commonly found on the lower limbs; nodules are palpable and may be accompanied by pain or tenderness; ulcers are often caused by ischemic necrosis due to vascular inflammation, frequently occurring on the extremities. These skin symptoms are characterized by diversity and recurrence.
2. Signs of multi-system involvement: Vasculitis can affect multiple systems, causing corresponding symptoms. If joints are involved, there may be joint pain and swelling; if the lungs are affected, symptoms such as coughing, chest tightness, and breathing difficulties may occur; if the kidneys are involved, hematuria and proteinuria may appear; if the nervous system is affected, symptoms like numbness, weakness, and pain in the limbs can occur. The simultaneous or sequential occurrence of abnormalities across multiple systems warrants suspicion of vasculitis.
3. Abnormal inflammatory indicators: Laboratory tests often reveal elevated inflammatory markers in patients with vasculitis, such as an increased erythrocyte sedimentation rate (ESR) and elevated C-reactive protein (CRP) levels. These indicators reflect the presence of an inflammatory response in the body. Although not specific, they provide important evidence for diagnosing vasculitis when combined with clinical symptoms. Additionally, abnormalities in white blood cell and platelet counts may also occur.
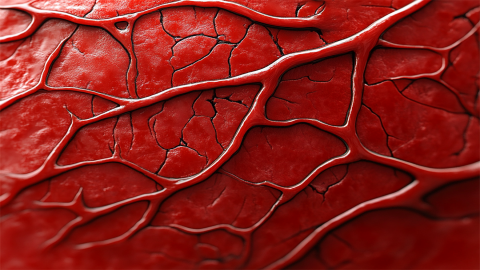
4. Vascular imaging changes: Examinations such as vascular ultrasound, CT angiography, and MRI angiography can reveal changes like thickened vascular walls, luminal narrowing, occlusion, or dilation. Different types of vasculitis affect different vascular regions; for example, large vessel vasculitis mainly affects the aorta and its branches, and imaging can show abnormal morphology of the corresponding vessels, providing direct diagnostic evidence.
5. Pathological biopsy results: Histopathological examination of the affected tissue is a key basis for diagnosing vasculitis. Characteristic findings include inflammatory cell infiltration in the vessel wall, vascular necrosis, and thrombus formation. Different types of vasculitis exhibit distinct pathological features; for example, leukocytoclastic vasculitis shows perivascular infiltration of neutrophils accompanied by nuclear fragmentation. Pathological examination helps determine the specific type of vasculitis.
When assessing whether a condition is vasculitis, it is essential to integrate and analyze the above-mentioned multiple factors rather than relying on a single criterion. In daily life, if symptoms suggestive of vasculitis appear, careful observation of symptom changes and timely completion of relevant investigations are important for accurate diagnosis.







