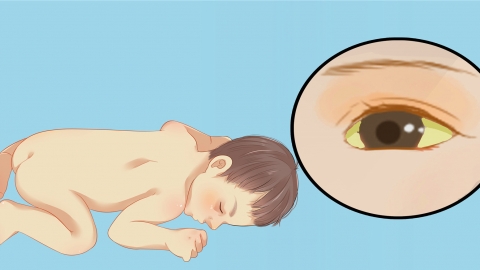
What causes hemolytic jaundice?
Generally, hemolytic jaundice may be caused by neonatal physiological hemolysis, congenital defects of the red blood cell membrane, autoimmune hemolytic anemia, infections, blood transfusions with incompatible blood types, and other factors. If experiencing any discomfort, timely medical consultation is recommended. Detailed explanations are as follows:
1. Neonatal Physiological Hemolysis
After birth, newborns have a relatively high number of red blood cells, which have short lifespans. When red blood cells are destroyed, the bilirubin produced exceeds the liver's metabolic capacity, leading to hemolytic jaundice. This condition typically does not require specific treatment. Parents can increase the frequency of feeding to promote bowel movements and assist in bilirubin excretion. Close monitoring of skin jaundice changes in the newborn is necessary. The jaundice usually appears 2-3 days after birth and can resolve spontaneously around 7-10 days.
2. Congenital Red Blood Cell Membrane Defects
When there is a congenital defect in the red blood cell membrane, red blood cells are prone to rupture, leading to increased red blood cell destruction and the release of large amounts of bilirubin, causing hemolytic jaundice. Daily care should focus on avoiding trauma and infections in the child to reduce triggers of red blood cell destruction. Regular blood tests, including complete blood count and bilirubin levels, should be conducted to monitor disease progression. If the condition is severe, blood transfusions or other treatments under a physician's guidance may be necessary.
3. Autoimmune Hemolytic Anemia
Autoimmune hemolytic anemia occurs when the body produces antibodies against its own red blood cells, leading to their destruction and excessive bilirubin production, resulting in hemolytic jaundice. Symptoms may include anemia and fatigue. Under a physician's guidance, glucocorticoids such as prednisone tablets or methylprednisolone tablets can be used to suppress the immune response. If hormone therapy proves ineffective, immunosuppressants such as cyclophosphamide tablets may be used. Adequate rest should be ensured, fatigue avoided, and nutrition supplemented with protein, iron, and other essential nutrients.
4. Infections
Certain infections, such as malaria and Epstein-Barr virus (EBV) infection, can damage red blood cells, leading to extensive destruction and resulting in hemolytic jaundice. Symptoms may include fever and chills. If malaria is diagnosed, antimalarial drugs such as artesunate-piperaquine tablets or chloroquine phosphate tablets can be administered under a physician's guidance. For EBV infection, antiviral medications such as acyclovir tablets or ganciclovir capsules may be used. Appropriate isolation measures should be taken to prevent cross-infection, and adequate hydration should be ensured.
5. Incompatible Blood Transfusion
If the blood type is incompatible during a blood transfusion, the recipient's antibodies attack and destroy the transfused red blood cells, causing severe hemolysis and the release of large amounts of bilirubin, resulting in hemolytic jaundice. Symptoms may include chills, high fever, and back pain. Once an incompatible blood transfusion occurs, the transfusion must be stopped immediately, and fluid replacement therapy should be initiated under a physician's guidance. Intravenous infusions of normal saline or glucose injections may be administered to maintain blood volume. Diuretics such as furosemide injection can be used to promote bilirubin excretion, and in severe cases, exchange transfusion therapy may be necessary.
In daily life, maintaining good personal hygiene to prevent infections, eating a balanced diet to ensure adequate nutrition and enhance immunity, and strictly following blood type compatibility principles during blood transfusions to reduce transfusion risks are recommended.








