What causes the formation of café-au-lait macules?
Generally, the formation of acquired dermal melanocytosis (ADM) may be caused by factors such as genetic influences, hormonal changes during puberty, post-inflammatory hyperpigmentation, melasma combined with pigmentation, or involvement of nevus of Ota. It is recommended to seek timely medical consultation, identify the underlying cause, and undergo symptomatic treatment under a physician's guidance. Detailed analysis is as follows:
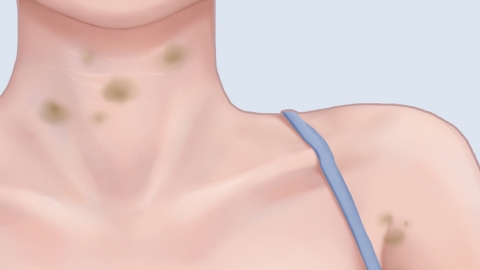
1. Genetic Influences: A family history of ADM may indicate genetic predispositions leading to abnormal melanocyte function, causing abnormal melanin deposition in the dermal layer of the skin and resulting in ADM, which typically appears during adolescence. Practicing daily sun protection helps prevent ultraviolet radiation from worsening pigmentation and reduces the risk of darkening of the pigmented spots.
2. Hormonal Changes During Puberty: Rapid fluctuations in estrogen and progesterone levels during puberty may stimulate increased melanocyte activity, promoting excessive melanin secretion and deposition in the skin, which can trigger ADM. Maintaining a regular sleep schedule, avoiding late nights, and reducing intake of high-sugar and high-fat foods are recommended.
3. Post-inflammatory Hyperpigmentation: Skin conditions such as eczema or dermatitis may lead to increased melanocyte activity after inflammation subsides, causing excessive melanin production and deposition, forming pigmented spots similar to ADM, often accompanied by a history of skin redness and itching. Patients may apply medications such as hydroquinone cream, azelaic acid cream, or retinoic acid cream as directed by a physician to inhibit melanin production.
4. Melasma Combined with Pigmentation: Long-term ultraviolet exposure or endocrine disorders may cause melasma. If left untreated, further melanin deposition in melasma areas may lead to ADM-like pigmentation changes, accompanied by symmetrically distributed light brown patches on the face. Under medical guidance, patients may use medications such as tranexamic acid tablets, vitamin C tablets, or glutathione tablets to improve symptoms.
5. Involvement of Nevus of Ota: Nevus of Ota is a dermal melanocytosis disorder. If the lesion expands to involve areas such as the zygomatic and temporal regions, it may present with an appearance similar to ADM, with colors typically appearing as bluish-gray or gray-brown. Treatments such as Q-switched laser therapy or picosecond laser therapy can be used to break up dermal melanin particles with laser energy, promoting their metabolic elimination.
In daily life, avoid frequent use of irritating skincare products or cosmetics to reduce skin friction and irritation. In the diet, appropriately increasing intake of foods rich in vitamin C and vitamin E, such as oranges, kiwifruit, and nuts, can help improve skin pigmentation status and maintain skin health.






