How to treat scabies
Normally, scabies may be caused by factors such as poor personal hygiene, close contact infection, simple scabies, scabious nodules, secondary bacterial infection, and others. It is recommended to seek timely medical attention, clarify the condition, and under a doctor's guidance, improve through daily care and medication. Detailed analysis is as follows:
1. Poor Personal Hygiene: Inadequate skin cleansing makes it easy for scabies mites to parasitize and reproduce in skin folds such as between fingers and armpits, causing itching and small, pale red papules. Take warm water baths daily, dry thoroughly after cleaning, and wash and sun-dry (for 1-2 hours) changed clothes and bedding in hot water to kill residual mites and reduce the possibility of repeated infections.
2. Close Contact Infection: Direct skin contact with a scabies patient or using items previously used by the patient, such as towels, bed sheets, and clothing, can easily lead to scabies mite infection. Temporary isolation from the patient is necessary. The patient's personal items should be washed and disinfected separately, and healthy individuals should promptly wash their hands with soap after contact with the patient to prevent cross-infection.
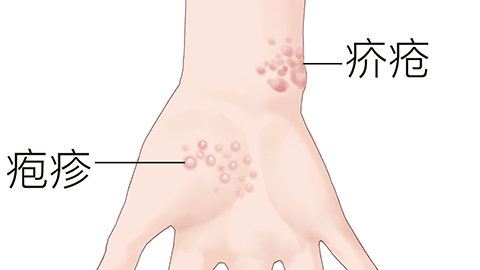
3. Simple Scabies: After scabies mites bite the skin and release toxins, localized inflammation occurs, presenting as burrow-like rashes accompanied by severe itching at night. Follow medical advice to apply topical medications such as sulfur ointment, lindane cream, or crotamiton cream. Apply the medication over the entire body according to the prescribed course, especially paying attention to hidden areas such as wrists and groin. Avoid bathing and changing clothes during application.
4. Scabious Nodules: If simple scabies isn't treated promptly, inflammation worsens, forming pea-sized hard nodules on the skin with more intense itching. Follow medical advice to apply topical corticosteroid creams such as hydrocortisone butyrate cream, mometasone furoate cream, or halometasone cream, or consider cryotherapy, which uses low temperatures to destroy nodule tissues and relieve itching and nodule symptoms.
5. Secondary Bacterial Infection: Skin damage caused by intense scratching allows bacterial invasion, such as Staphylococcus aureus, leading to pustules, redness, and pain. Follow medical advice to apply topical antibiotics such as mupirocin ointment, fusidic acid cream, or compound polymyxin B ointment to control infection and prevent inflammation from spreading.
In daily life, keep fingernails trimmed regularly to avoid scratching and worsening skin damage. Maintain a light diet and reduce the intake of spicy or irritating foods. Keep the living environment ventilated and dry, and regularly wipe furniture with chlorine-containing disinfectants. Comprehensive care can promote recovery and maintain skin health.





