Is ankylosing spondylitis very painful?
Generally speaking, whether ankylosing spondylitis causes significant pain depends on factors such as the disease stage, severity, and individual differences. If discomfort occurs, timely medical consultation is recommended. Detailed analysis is as follows:
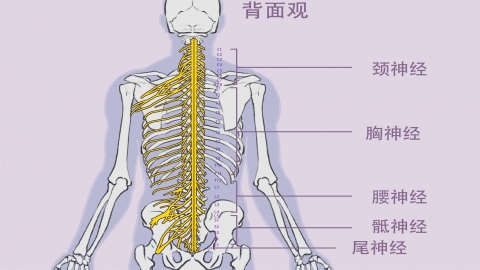
If ankylosing spondylitis reaches the middle or late stages with severe inflammation infiltration in the spine and sacroiliac joints, damage to joint cartilage, bone spurs, or even joint ankylosis, and the patient has a high sensitivity to pain, significant pain usually occurs. The pain is primarily concentrated in the lower back and may extend to the buttocks and upper thighs, presenting as persistent or intermittently worsening pain that intensifies with activity. Some individuals may experience severe nighttime pain that affects sleep quality.
If ankylosing spondylitis is in its early stage with mild severity, the inflammation may only slightly irritate the joints and surrounding tissues. If the patient has a high tolerance for pain, mild inflammatory stimulation may not provoke noticeable symptoms. Pain might manifest only as occasional backache or stiffness, which may ease with rest or activity and is easily overlooked, leading to delayed diagnosis.
When symptoms such as lower back pain and stiffness appear, timely medical evaluation is necessary to determine the disease stage. Avoid maintaining the same posture for prolonged periods in daily life, and engage in appropriate spinal stretching exercises and swimming to maintain joint flexibility. During pain episodes, apply heat therapy and take analgesics as directed by a physician; self-adjustment of dosage is not recommended. Regular follow-up assessments of inflammatory markers and imaging studies are essential to monitor disease progression and adjust treatment plans accordingly.




