失血性休克是What发病机制
Generally, the core pathophysiological mechanisms of hemorrhagic shock include a rapid decrease in blood volume, inadequate effective circulation perfusion, tissue hypoxia and ischemia, metabolic imbalance, and multi-organ dysfunction. A detailed analysis is as follows:
1. Rapid reduction in blood volume: Significant blood loss directly leads to insufficient circulating blood volume. The total amount of blood within the vascular system fails to meet the body's demands, resulting in decreased venous return and compromised cardiac pumping function, triggering a cascade of subsequent reactions.
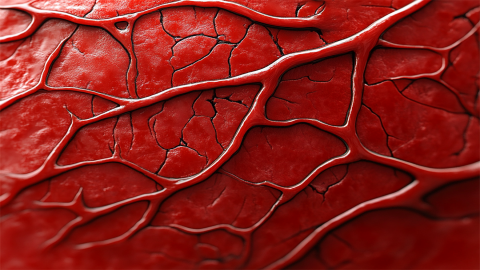
2. Inadequate effective perfusion: Following reduced blood volume, decreased blood pressure leads to lower perfusion pressure. Vital organs and peripheral tissues cannot receive sufficient blood supply, causing slowed microcirculatory flow, which may even become stagnant or cease entirely.
3. Tissue hypoxia and ischemia: Blood is the primary carrier of oxygen and nutrients; thus, poor perfusion directly results in tissue hypoxia. Cells are deprived of adequate oxygen for metabolism, leading to enhanced anaerobic metabolism and accumulation of acidic byproducts such as lactic acid.
4. Metabolic disturbances and imbalances: Anaerobic metabolism due to hypoxia causes acid-base imbalance, resulting in metabolic acidosis. Concurrent electrolyte disturbances, such as hyperkalemia, further impair normal cardiac function and neuromuscular activity.
5. Multi-organ dysfunction: Prolonged ischemia and hypoxia damage critical organs including the heart, brain, kidneys, and lungs. Myocardial ischemia reduces contractility, cerebral ischemia leads to altered consciousness, and renal ischemia results in acute kidney injury, potentially culminating in multiple organ failure.
Clinically, early recognition of signs of hemorrhagic shock is essential, with immediate initiation of emergency interventions such as hemostasis and fluid resuscitation. Continuous monitoring of vital signs and organ function during treatment allows timely adjustments to the therapeutic plan, reducing the risk of multi-organ damage.








