What does HPV 1651 positive mean, and is it serious?
Generally, a positive result for HPV types 16 and 51 indicates infection with human papillomavirus (HPV) types 16 and 51. Among these, type 16 is a high-risk subtype that requires particular attention. However, the severity of the condition must be determined based on cervical lesion examination results. If concerned, it is recommended to seek medical consultation promptly. Detailed analysis is as follows:
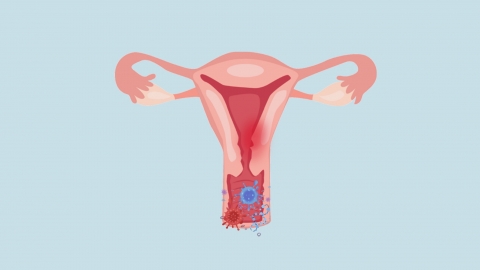
HPV type 16 is a high-risk subtype strongly associated with an increased risk of cervical lesions and closely linked to the development of cervical cancer. HPV type 51 is also classified as a high-risk subtype, although its pathogenic risk is relatively lower than that of type 16. A positive result for both subtypes indicates the presence of a high-risk HPV infection, but this does not directly mean the individual has cancer. Most infected individuals can clear the virus naturally through their immune system within 1–2 years, while only a small number with persistent infections may develop cervical lesions.
The severity of the condition should be further evaluated through cervical TCT (thin-prep cytology test) or colposcopy. If no cervical cell abnormalities are found, this suggests there is currently no significant lesion, and regular follow-up examinations are sufficient. If abnormal cells or mild, moderate, or severe lesions are detected, corresponding interventions should be implemented according to the degree of lesion. More severe lesions require more aggressive management, but with timely intervention, the prognosis is generally favorable.
After diagnosis, patients should follow medical advice to complete relevant cervical lesion evaluations and clarify their disease status; undergo regular follow-up testing for HPV and cervical health to monitor viral clearance or changes in lesions; maintain regular sleep patterns and a balanced diet to strengthen immunity and support viral clearance; avoid excessive anxiety, actively cooperate with medical monitoring and treatment, and reduce the risk of disease progression.




