Can salpingitis be detected by transvaginal ultrasound?
In general, whether salpingitis can be detected by transvaginal ultrasound depends on the specific condition of the inflammation. If there are any discomforts, it is recommended to seek medical attention promptly. The detailed analysis is as follows:
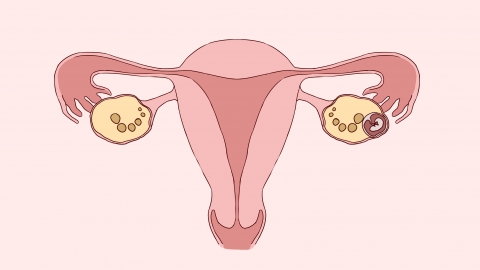
During acute salpingitis, transvaginal ultrasound can often detect abnormalities. Inflammation causes congestion and edema of the fallopian tubes, leading to tubal dilation with possible fluid or pus accumulation inside. On ultrasound imaging, the fallopian tubes may appear thickened and irregular in shape, with increased and uneven echogenicity in surrounding tissues. In some cases, hypoechoic (fluid-filled) areas within the tube may also be observed. Combined with clinical symptoms, this helps support the diagnosis of inflammation.
In mild cases of chronic salpingitis where significant structural changes have not occurred, transvaginal ultrasound may fail to detect the condition. At this stage, there might only be slight adhesions or mucosal inflammation without obvious thickening or fluid accumulation. These subtle changes make it difficult to distinguish the affected tubes from normal ones on ultrasound images, increasing the risk of missed diagnosis.
Prior to the examination, maintain external genital hygiene and avoid sexual intercourse and vaginal medications to minimize interference with test results. Ultrasound findings should be interpreted in conjunction with clinical symptoms, complete blood count, vaginal discharge tests, and other relevant examinations. A definitive diagnosis should not rely solely on ultrasound results. If symptoms such as lower abdominal pain or abnormal vaginal discharge occur, prompt medical evaluation is advised, and a healthcare provider will determine an appropriate diagnostic approach.




