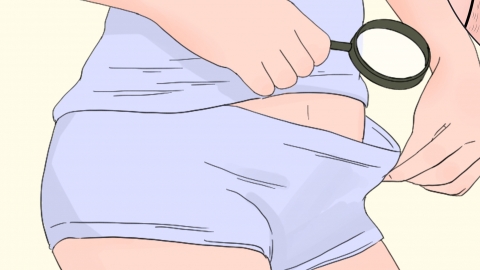
What causes whitening on the inner labia, and what should be done about it?
Generally, whitening on the inner labia may be related to hormonal fluctuations, local friction or irritation, vulvar leukoplakia, vulvovaginal candidiasis, or lichen sclerosus. It is recommended to seek medical advice promptly to determine the underlying cause and, under a doctor's guidance, improve the condition through daily care, medications, or surgical treatments as appropriate. Detailed explanations are as follows:
1. Hormonal fluctuations: During puberty, pregnancy, or perimenopause, unstable estrogen levels can reduce local pigment production, causing the mucosa to become lighter in color with uniform pale white patches. Maintain a regular sleep schedule, avoid staying up late, drink 300ml of unsweetened soy milk daily or consume 50g of tofu to increase intake of phytoestrogens.
2. Local friction or irritation: Wearing synthetic fiber underwear for prolonged periods, cycling, or frequent sexual activity can repeatedly compress the mucosa, leading to thickened keratin layers, reduced blood flow, lightened color, and mild flaking. Immediately switch to loose cotton underwear, avoid cycling and vigorous sexual activity, and apply a cold towel gently for 1–2 minutes after washing with warm water before bedtime to reduce friction-induced congestion and promote mucosal recovery.
3. Vulvar leukoplakia: Chronic irritation and immune abnormalities lead to depigmentation of the vulvar mucosa, resulting in ill-defined milky white patches on the inner labia, often accompanied by itching or burning. Patients may use topical medications such as hydrocortisone butyrate cream, tacrolimus ointment, or clobetasol propionate cream as directed by a physician to reduce inflammation and promote repigmentation.
4. Vulvovaginal candidiasis: Overgrowth of *Candida albicans* leads to increased secretions that adhere to the mucosa, forming white membrane-like deposits. When wiped away, they reveal a red, moist base and are typically associated with significant itching. Patients may use antifungal medications such as clotrimazole vaginal tablets, miconazole nitrate suppositories, or nystatin vaginal suppositories as prescribed to suppress fungal growth and alleviate whitening symptoms.
5. Lichen sclerosus: Autoimmune abnormalities cause collagen degeneration in the mucosa, resulting in porcelain-white atrophic patches with a shiny surface, possibly accompanied by fissures or dyspareunia. When topical medications are ineffective or adhesions develop, CO₂ laser ablation may be performed to remove the affected layer and stimulate collagen remodeling. In cases of severe scarring, vulvar reconstructive surgery can be considered to release adhesions, restore normal anatomy, and improve both function and appearance.
In daily life, avoid using alkaline cleansers; opt for gentle washing with plain water. Reduce consumption of spicy foods, maintain regular bowel movements, and adopt comprehensive hygiene practices to support mucosal recovery and maintain overall vulvar health.





