What is the difference between rectal prolapse and internal hemorrhoids?
Although both rectal prolapse and internal hemorrhoids may present with anal protrusions, they differ significantly in terms of affected site, appearance of the protrusion, characteristics of bleeding during bowel movements, accompanying symptoms, and progression of severity. The specific differences are as follows:
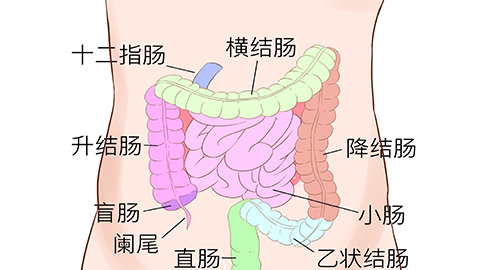
1. Affected Site: Internal hemorrhoids occur beneath the mucosa at the distal end of the rectum above the dentate line. They result from varicose enlargement of the hemorrhoidal venous plexus, forming soft masses located relatively deep within the anal canal. In early stages, the protruding tissue typically consists of hemorrhoidal nodules. Rectal prolapse, on the other hand, involves the protrusion of the rectal mucosa or full-thickness rectal wall. The displaced tissue originates from the rectal wall itself and is located more distally, potentially involving the distal rectum or even part of the sigmoid colon.
2. Appearance of Protrusion: The protrusion in internal hemorrhoids usually appears as one or more soft, round or oval hemorrhoidal nodules, bright red or dark red in color, with a smooth surface and soft texture. If reducible, their shape remains largely unchanged after repositioning. In contrast, the protrusion in rectal prolapse consists of rectal mucosa or intestinal tube, appearing cylindrical or ring-shaped with circular folds (rugae), pale red or pink in color, and firmer in texture. The extent of tissue protrusion is generally greater than that seen in internal hemorrhoids.
3. Characteristics of Bleeding: Bleeding is common in internal hemorrhoids, typically presenting as fresh red blood dripping during defecation or staining toilet paper. The blood does not mix with stool and often occurs alongside prolapsed hemorrhoidal nodules. In rectal prolapse, bleeding is less common and only occurs when the mucosa of the prolapsed tissue becomes damaged, resulting in minimal spotting with lighter-colored blood.
4. Accompanying Symptoms: Besides prolapse and bleeding, internal hemorrhoids are often associated with sensations of anal heaviness and itching. Severe pain may occur if the hemorrhoidal nodule becomes incarcerated. Rectal prolapse primarily causes feelings of incomplete evacuation and anal heaviness. If the prolapsed tissue cannot be reduced, complications such as mucosal edema and erosion may develop.
5. Progression of Severity: In early-stage internal hemorrhoids, the prolapsed tissue can spontaneously reduce; in later stages, manual reduction is required, and in severe cases, it cannot be reduced at all. In early rectal prolapse, protrusion occurs only during defecation, but as the condition progresses, it may happen during walking or coughing. In severe cases, full-thickness rectal wall prolapses and cannot be reduced, potentially leading to anal sphincter relaxation.
When an anal protrusion occurs, initial differentiation based on the above features is helpful, but a definitive diagnosis requires medical evaluation through professional examination. Regardless of whether the diagnosis is rectal prolapse or internal hemorrhoids, early treatment is essential to prevent worsening symptoms and impairment of quality of life. During treatment, maintaining regular bowel movements and avoiding straining during defecation are crucial.






