What should I do if I get hives when exposed to cold or heat?
Generally, developing urticaria upon exposure to cold or heat may be caused by sudden temperature changes, a weakened skin barrier, cold-induced urticaria, heat-induced urticaria, or autoimmune urticaria. It is recommended to seek medical attention promptly, identify the underlying cause, and then improve symptoms under a doctor's guidance through general management, medication, and other approaches. A detailed analysis is as follows:
1. Sudden temperature change stimulation: Rapid alternation between cold and heat causes abrupt constriction and dilation of skin blood vessels, activating mast cells to release histamine and resulting in hives. Take protective measures when going outdoors—wear sun hats in summer and scarves and gloves in winter. Avoid moving suddenly from hot environments into air-conditioned rooms or cold outdoor areas to minimize thermal shock.
2. Weakened skin barrier: Over-cleansing or frequent use of exfoliating products can damage the skin’s protective layer, making it more susceptible to allergic reactions triggered by temperature changes. Discontinue use of soap-based cleansers and exfoliants, switch to moisturizers containing ceramides, limit facial cleansing to no more than twice daily, and maintain facial water temperature at 32–35°C.
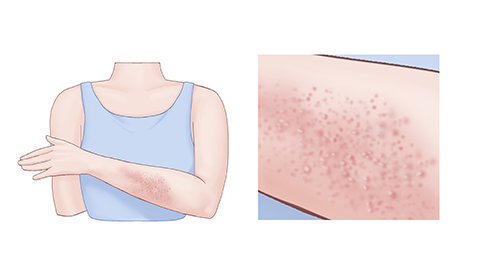
3. Cold-induced urticaria: Triggered by exposure to cold air or cold water, this condition causes itchy hives, commonly appearing on the face and hands. Avoid washing with cold water and reduce outdoor activities in cold weather. Follow medical advice to take oral medications such as loratadine tablets, cetirizine hydrochloride tablets, or ebastine tablets.
4. Heat-induced urticaria: Occurs after exposure to temperatures above 43°C or intense physical activity, causing small, stinging hives in affected areas. Avoid saunas and hot baths, cool down and rehydrate promptly after exercise, and take medications as directed by a physician, such as fexofenadine hydrochloride tablets, desloratadine dry suspension, or levocetirizine oral solution.
5. Autoimmune urticaria: In this condition, autoantibodies attack mast cells, with temperature changes acting only as triggers. Hives recur frequently and last longer. Maintain regular sleep patterns, avoid staying up late, strengthen immunity, and follow medical instructions to use medications such as prednisone tablets, methylprednisolone tablets, or cyclosporine soft capsules.
In daily life, avoid spicy foods, seafood, and other allergenic foods. Eat more fresh fruits and vegetables rich in vitamins. Wear loose, breathable cotton clothing to reduce skin friction. Keep a record of urticaria episodes to identify specific triggers and take targeted steps to avoid them, helping to reduce the frequency of outbreaks.




