What does it mean when psoriasis feels hard to the touch?
In general, the hardening of psoriatic skin may be caused by factors such as dryness and dehydration, thickened stratum corneum, disease progression, local inflammatory stimulation, or improper use of topical medications. It is recommended to seek medical attention promptly to determine the exact cause. The specific analysis is as follows:
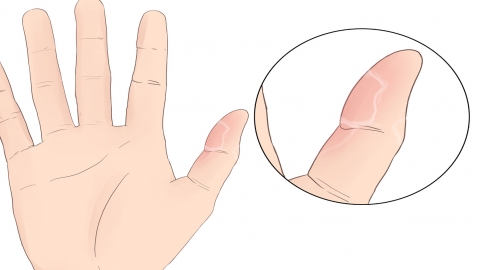
1. Skin dryness and dehydration: Patients with psoriasis have a fragile skin barrier. Dry environments or inadequate moisturization can lead to rapid water loss, causing the stratum corneum to become dry and hardened. Daily intensive moisturizing is essential—choose emollients containing petroleum jelly or ceramides, and avoid frequent washing with hot water.
2. Thickened stratum corneum: Psoriasis accelerates keratinocyte proliferation while impairing normal shedding, leading to accumulation and thickening of the stratum corneum, which makes lesions feel harder. Under physician evaluation, mild keratolytic agents used in combination with moisturizers can help promote normal desquamation.
3. Disease progression and worsening: During the progressive phase of psoriasis, inflammation intensifies, keratinocyte proliferation speeds up, and lesions become harder, often accompanied by expanding erythematous plaques and increased itching. After diagnosis, doctors may prescribe topical treatments such as calcipotriol ointment, tazarotene gel, or desonide cream to control inflammation. Medications must be used strictly as directed.
4. Local inflammatory stimulation: Prolonged inflammation in psoriatic lesions can lead to tissue hyperplasia and fibrosis, resulting in hardened texture, possibly accompanied by mild pain or burning sensation. Following medical assessment, systemic therapies such as acitretin capsules, methotrexate tablets, or cyclosporine soft capsules may be prescribed to modulate the immune response and reduce inflammation.
5. Irritation from inappropriate topical medications: Long-term use of harsh topical agents can cause skin dryness and abnormal thickening of the stratum corneum, leading to harder lesions and increased scaling. Discontinue any suspected irritant drugs immediately. A doctor should adjust the treatment plan, switching to milder medications and incorporating moisturizers to relieve symptoms.
In daily life, avoid scratching affected areas and wear loose, cotton clothing. Maintain a light diet rich in vitamin-containing foods. If lesion hardness increases or is accompanied by discomfort, seek medical care promptly and strictly follow prescribed treatment regimens.




