Can patients with appendicitis take painkillers?
Whether patients with appendicitis can take analgesics depends on the stage of the disease and diagnostic results. Patients with confirmed diagnosis and no contraindications may take analgesics under a doctor's guidance. However, self-medication with analgesics is not recommended when the condition hasn't been diagnosed or there is a risk of acute or severe illness. If any abnormalities occur, prompt medical attention is advised. Detailed explanations are as follows:
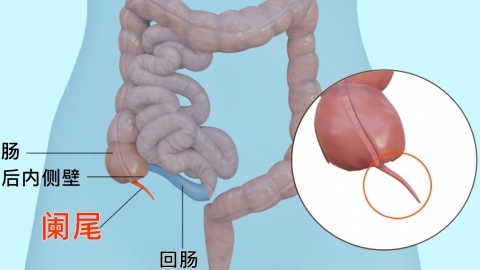
If a patient has been diagnosed with appendicitis through examinations such as ultrasound and routine blood tests, and there are no acute or severe conditions like appendiceal perforation or intra-abdominal bleeding, analgesics may be taken under a doctor's guidance. For example, ibuprofen sustained-release capsules can relieve mild to moderate abdominal pain by inhibiting prostaglandin synthesis. The usual dosage is 0.3 grams each time, every 12 hours. However, these medications should be taken after meals to reduce gastrointestinal irritation.
Patients with appendicitis who have not yet received a definitive diagnosis or who are at risk of complications such as appendiceal perforation or suppurative peritonitis must not take analgesics on their own. Painkillers may mask typical symptoms such as the severity of abdominal pain and the area of tenderness, making it difficult for doctors to accurately assess disease progression, delaying surgical timing, and even leading to severe complications such as septic shock. Additionally, patients allergic to nonsteroidal anti-inflammatory drugs (NSAIDs) or with a history of gastrointestinal ulcers should also avoid these medications.
Appendicitis patients experiencing abdominal pain should seek immediate medical attention to clarify their condition and strictly follow medical advice regarding medication. Self-administration of analgesics is strongly discouraged.