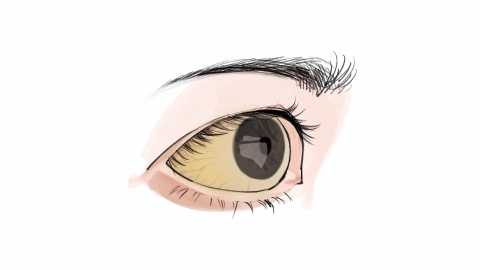
What causes pathological jaundice?
Generally, pathological jaundice in newborns may be caused by factors such as immature liver development, components in breast milk, polycythemia, viral hepatitis, or biliary obstruction. If any discomfort occurs, prompt medical attention is recommended. Detailed explanations are as follows:
1. Immature Liver Development
In newborns, the enzyme systems involved in bilirubin metabolism within the liver are not yet fully developed, leading to weak bilirubin uptake and conversion capacity. This can result in bilirubin accumulation in the body and cause pathological jaundice. It is important to increase feeding frequency to promote bilirubin excretion through frequent bowel movements. Under a doctor's guidance, appropriate sun exposure (avoiding peak sunlight hours) can be used to help break down bilirubin with natural light. Regular monitoring of transcutaneous bilirubin levels and observation of skin jaundice changes are also necessary.
2. Influence of Breast Milk Components
Certain components in breast milk may inhibit bilirubin metabolism in a newborn's liver, increasing enterohepatic circulation of bilirubin and causing persistent jaundice. Typically, the infant continues to feed normally and remains in good spirits. If bilirubin levels do not exceed treatment thresholds, breastfeeding can continue, with gentle back patting after each feeding to aid digestion. If jaundice continues to worsen, breastfeeding should be temporarily stopped for 2-3 days under medical guidance, switching to formula feeding. During this time, a breast pump should be used to maintain milk production, and breastfeeding can resume once jaundice subsides.
3. Polycythemia
When a newborn has an excessive number of red blood cells, bilirubin produced from red blood cell breakdown may exceed the liver's metabolic capacity, leading to jaundice. This may be accompanied by symptoms such as a ruddy complexion and increased blood volume. Under medical guidance, partial exchange transfusion may be used to reduce red blood cell count, along with albumin injections to bind free bilirubin. Blood routine tests and bilirubin levels should be closely monitored during treatment, while maintaining fluid balance and avoiding dehydration.
Hepatitis virus infection can damage liver cells, affecting bilirubin metabolism and excretion, thereby causing jaundice. Symptoms may include hepatomegaly and abnormal liver function. Under medical guidance, antiviral medications such as recombinant human interferon α1b injection, lamivudine oral solution, and adefovir dipivoxil tablets may be used to inhibit viral replication. Hepatoprotective drugs such as reduced glutathione injection may also be administered to promote liver cell repair. Strict adherence to prescribed medication and regular liver function follow-ups are essential during treatment.
5. Biliary Obstruction
Biliary obstruction prevents normal bile excretion, causing bilirubin to reflux into the bloodstream and resulting in jaundice. The more severe the obstruction, the deeper the jaundice may become. Symptoms may include lighter-colored stools and darker urine. Early imaging tests should be conducted to identify the site of obstruction, and under medical guidance, ursodeoxycholic acid capsules may be used to promote bile secretion. Surgery may be required to relieve the obstruction when necessary. Postoperative monitoring of stool color and jaundice changes is important, along with maintaining wound cleanliness to prevent infection.
In daily life, it is important to keep the newborn's skin clean and avoid contact with infection sources. Mothers who breastfeed should maintain a light diet and avoid spicy or stimulating foods.







