Is gastrointestinal bleeding in elderly people serious?
Generally speaking, the severity of gastrointestinal bleeding in elderly individuals depends on factors such as the volume and rate of bleeding, as well as their baseline health status. If any discomfort occurs, prompt medical attention is recommended. Detailed analysis is as follows:
If the volume of gastrointestinal bleeding in the elderly is small, with black tarry stools as the only symptom and no vomiting of blood, slow bleeding rate, and absence of symptoms such as dizziness, palpitations, or weakness, along with no severe underlying conditions like hypertension, diabetes, or heart disease, and adequate compensatory capacity of the body, the condition is usually not severe. Prompt medical evaluation to identify the cause and appropriate treatment typically allows for rapid control of the bleeding, with minimal overall impact on health.
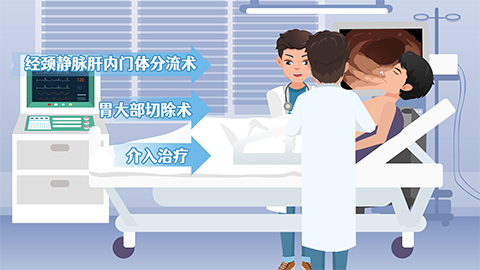
If the volume of gastrointestinal bleeding in the elderly is large, with massive vomiting of blood or passage of blood in stool, rapid bleeding rate, accompanied by symptoms such as pallor, altered consciousness, or decreased blood pressure indicating pre-shock or shock states, or if the individual has underlying severe cardiopulmonary diseases, cirrhosis, or malignancies and poor physical tolerance, the condition is generally severe. Significant blood loss can rapidly exacerbate existing conditions and even threaten life, necessitating immediate emergency treatment.
After gastrointestinal bleeding occurs in elderly individuals, food and fluid intake should be stopped immediately. The affected person should remain lying down to rest and avoid physical activity that could worsen the bleeding. Emergency medical services should be contacted promptly, and detailed information regarding the patient's medical history, medication use, and specifics of the bleeding episode should be provided to the doctors upon arrival. Strict adherence to medical instructions is essential during treatment, and self-adjustment of medications or diet should be avoided. After stabilization of the condition, regular follow-up evaluations are necessary to closely manage underlying diseases, and dietary adjustments should focus on bland, easily digestible foods to reduce irritation to the gastric mucosa.










