Can a fundoscopic examination detect retinal detachment?
In most cases, routine fundus examinations can detect retinal detachment. However, if the detachment is very small or located in a hidden area, more detailed tests may be required for accurate diagnosis. If there are concerns, it is recommended to seek medical advice promptly. Detailed analysis is as follows:
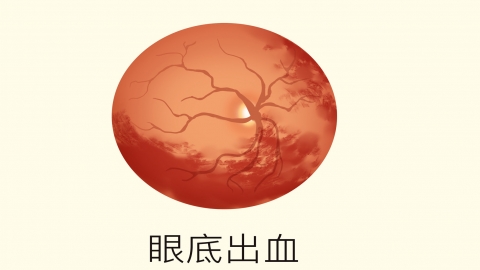
When conventional methods such as dilated fundus examination or ophthalmoscopy are used, retinal detachments with clearly visible areas can be easily identified. These methods allow clear observation of the detached region, severity, and whether complications such as retinal tears or hemorrhage are present. This enables rapid and definitive diagnosis, providing essential information for determining subsequent treatment plans—such scenarios are commonly encountered in clinical practice.
If retinal detachment is in its early stage, involves only a very small area, or occurs in the peripheral regions of the fundus, routine fundus examinations may fail to clearly capture the abnormal signs, increasing the risk of missed diagnosis. In such cases, more advanced imaging techniques—such as optical coherence tomography (OCT) or fundus angiography—are necessary to accurately identify subtle structural changes in the retina and confirm the presence of early-stage detachment.
Prompt fundus examination is essential if symptoms such as floating shadows, flashes of light, or visual field defects occur. Prior to examination, proper pupil dilation should be performed as instructed to ensure adequate visualization. Once diagnosed, timely treatment is crucial to prevent progression of the detachment and preserve vision.





