What should I do if a wound becomes inflamed?
Generally, wound inflammation may be caused by improper wound management, poor local blood circulation, skin and soft tissue infection, Staphylococcus aureus infection, diabetic foot, or other reasons. General treatment, medication, and other measures can be taken to improve the condition. It is important to seek medical attention promptly and follow medical advice for treatment. The specific details are as follows:
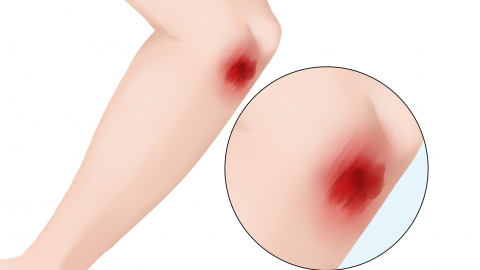
1. Improper wound management: After sustaining a wound, failure to promptly clean, disinfect, and dress the wound, or improper dressing techniques, may lead to bacterial invasion and proliferation, triggering an inflammatory response and resulting in redness and swelling. Immediate wound cleaning and disinfection should be performed using medications such as povidone-iodine solution or hydrogen peroxide solution. Appropriate dressing methods should be selected based on the wound condition, and the wound should be kept dry.
2. Poor local blood circulation: Poor blood circulation at the wound site can impede the healing process and increase the risk of inflammation. This may be caused by overly tight dressing, unfavorable wound location, or systemic circulatory disorders. The dressing method should be adjusted to avoid excessive tightness, thus promoting blood circulation.
3. Skin and soft tissue infection: Skin and soft tissue infections refer to inflammatory conditions of the skin and subcutaneous tissues, which can be caused by various pathogens, including bacteria, fungi, and others. When a wound becomes infected by pathogens, an inflammatory response occurs, causing rashes. Under a doctor's guidance, medications such as roxithromycin capsules, erythromycin ointment, and fusidic acid cream can be used for anti-infective and anti-inflammatory treatment.
4. Staphylococcus aureus infection: Staphylococcus aureus is a common pathogen causing skin infections. When wounds are exposed to unclean environments, they are prone to infection by this bacterium. Following Staphylococcus aureus infection, rapid bacterial proliferation and toxin production can trigger an inflammatory response, leading to intensified pain. Under medical guidance, medications such as amoxicillin capsules, levofloxacin hydrochloride capsules, and cefixime granules can be used for antibacterial and anti-inflammatory treatment.
5. Diabetic foot: Diabetic foot refers to foot ulcers, infections, and deep tissue damage in diabetic patients caused by distal lower limb nerve abnormalities and varying degrees of peripheral vascular disease. Due to decreased overall immunity and weakened wound healing capacity in diabetic patients, wound inflammation may occur alongside hyperglycemia. Under medical guidance, medications such as metformin hydrochloride tablets, pioglitazone hydrochloride tablets, and mecobalamin tablets can be used to lower blood glucose levels and promote nerve cell metabolism.
During the healing process, proper wound care and preventive measures should be emphasized to avoid re-injury and infection.








