Why does the uterus develop adhesions?
Normally, uterine adhesions may be caused by factors such as endometrial trauma, infection, low estrogen levels, genetic predisposition, and congenital uterine malformations. It is recommended to seek timely medical attention, identify the underlying cause, and receive symptomatic treatment under a doctor's guidance. Detailed analysis is as follows:
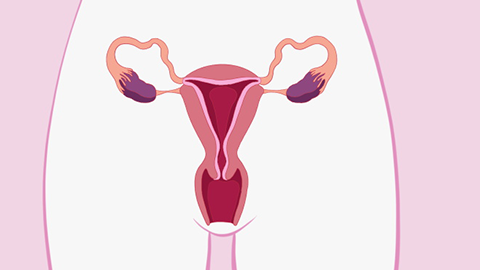
1. Endometrial trauma: Uterine cavity procedures such as induced abortion, curettage, and resection of uterine septum can damage the basal layer of the endometrium, leading to adhesion of the anterior and posterior walls or lateral walls of the uterus. This is commonly seen in individuals who have undergone multiple uterine cavity surgeries. Postoperatively, estradiol valerate tablets may be used under medical supervision to promote endometrial repair, and an intrauterine device can be placed to prevent adhesions. If adhesions have already formed, hysteroscopic adhesiolysis is required, followed by antibiotic use as directed to prevent infection.
2. Infection: Inflammatory stimuli such as endometritis and pelvic inflammatory disease can disrupt the normal structure of the endometrium, leading to increased inflammatory exudate and causing uterine adhesions, which may be accompanied by fever and lower abdominal pain. Patients should follow medical advice to use medications such as amoxicillin-clavulanate potassium tablets, ceftriaxone sodium injection, and doxycycline tablets to control the infection. If adhesions persist after the inflammation subsides, surgical separation is required.
3. Low estrogen levels: Estrogen promotes endometrial growth. When levels are too low, the endometrium's ability to repair is reduced, making uterine adhesions more likely. This is commonly seen in postmenopausal women or those with diminished ovarian function. Under medical supervision, conjugated estrogen tablets or nylestriol tablets can be used to supplement estrogen. Additionally, dietary adjustments should include increased intake of legumes, nuts, and other foods rich in phytoestrogens.
4. Genetic factors: Some patients have a genetic predisposition with poor endometrial repair capacity, making them prone to uterine adhesions even after minor injuries, and there may be similar cases in the family. These patients should especially avoid unnecessary intrauterine procedures. If adhesions occur, early hysteroscopic surgery is needed, followed by long-term postoperative follow-up.
5. Congenital uterine malformations: Congenital abnormalities such as uterine septum or bicornuate uterus can affect the normal structure and blood flow of the uterus, increasing the risk of endometrial injury and subsequently causing uterine adhesions, which may be accompanied by menstrual irregularities. These malformations can be corrected surgically, such as via hysteroscopic resection of the uterine septum, followed by sequential estrogen-progestin therapy postoperatively to promote endometrial recovery and prevent recurrence of adhesions.
In daily life, effective contraceptive measures should be taken to reduce uterine cavity procedures such as induced abortions. Personal hygiene should be maintained to avoid genital tract infections. If symptoms such as decreased menstruation, amenorrhea, or abdominal pain occur, timely medical evaluation is necessary for early detection and treatment of uterine adhesions to prevent impairment of fertility function.




