How should perianal abscess be drained?
Perianal abscess drainage typically involves several methods: surgical incision and drainage, puncture aspiration and drainage, incision with seton placement, tube drainage, or spontaneous rupture and drainage. Specific details are as follows:
1. Surgical Incision and Drainage: This is the most commonly used clinical method, suitable for cases where the abscess has fully formed and exhibits obvious fluctuation. The physician makes an incision at the weakest point of the abscess to drain the pus, removes necrotic tissue, and places a drainage strip to facilitate the discharge of subsequent secretions. This reduces the risk of infection spread and promotes healing.
2. Puncture Aspiration and Drainage: For deep-seated or small-volume abscesses, or when patients are temporarily unfit for surgery due to medical conditions, pus can be aspirated via needle puncture to relieve symptoms. A sterile needle is inserted into the abscess cavity to withdraw pus, temporarily reducing local pressure and pain. However, this method often leaves residual pus and usually requires additional follow-up treatment.
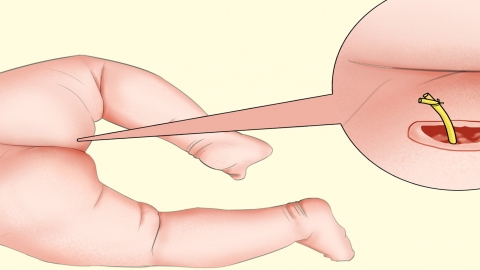
3. Incision with Seton Placement: For abscesses in special locations (e.g., near the anal sphincter), this technique is used to preserve anal function and prevent postoperative incontinence. After incising the abscess, a rubber band (seton) is threaded between the lesion and the anus. Through gradual cutting action over time, the seton facilitates continuous drainage while promoting tissue healing and minimizing functional damage.
4. Tube Drainage: For abscesses with thick pus or poor drainage, physicians may place a drainage tube after incision to ensure continuous outflow of pus and prevent re-accumulation due to premature closure of the abscess cavity. The tube must be regularly replaced until the cavity is completely clean and granulation tissue has formed, after which it can be removed to promote final healing.
5. Spontaneous Rupture and Drainage: Some abscesses may spontaneously rupture when they reach a certain stage, allowing pus to drain out and temporarily relieving local pain and swelling. However, the natural opening is often small and poorly positioned, leading to incomplete drainage. Residual pus may cause recurrent infections and potentially lead to the formation of an anal fistula, necessitating professional medical intervention.
Upon experiencing symptoms of perianal abscess, do not attempt self-squeezing or wait for spontaneous rupture. Prompt medical consultation is essential for proper evaluation and selection of appropriate drainage methods. During treatment, maintain cleanliness and dryness of the perianal area, avoid prolonged sitting and spicy foods, and follow medical advice for dressing changes and follow-up visits to ensure complete healing of the abscess cavity and prevent complications.